Learn practical ME/CFS tips including pacing, sleep, nutrition, and stress support, plus how functional medicine helps address root causes and triggers.
Living with Chronic Fatigue Syndrome, also known as Myalgic encephalomyelitis or ME/CFS, can feel like your body is running on a battery that never fully charges. It is not just “being tired.” It is a complex condition that can affect energy, sleep, cognition, pain levels, immune function, and how your body handles even small amounts of physical or mental effort.
Many people living with ME/CFS feel frustrated because rest alone does not improve symptoms, and pushing through fatigue often makes things worse. Understanding how this condition works and learning how to manage it safely is an important first step toward better stability and quality of life.
This guide explains what ME/CFS is, what commonly triggers flare-ups, and practical tips for pacing, sleep, nutrition, stress, and gentle movement.
Chronic Fatigue Syndrome, also known as Myalgic encephalomyelitis or ME/CFS, is a serious and long-term condition that affects how the body produces and recovers energy. It is not the same as everyday tiredness or burnout. People with ME/CFS experience fatigue that is deep, persistent, and disabling, often interfering with work, relationships, and basic daily activities.
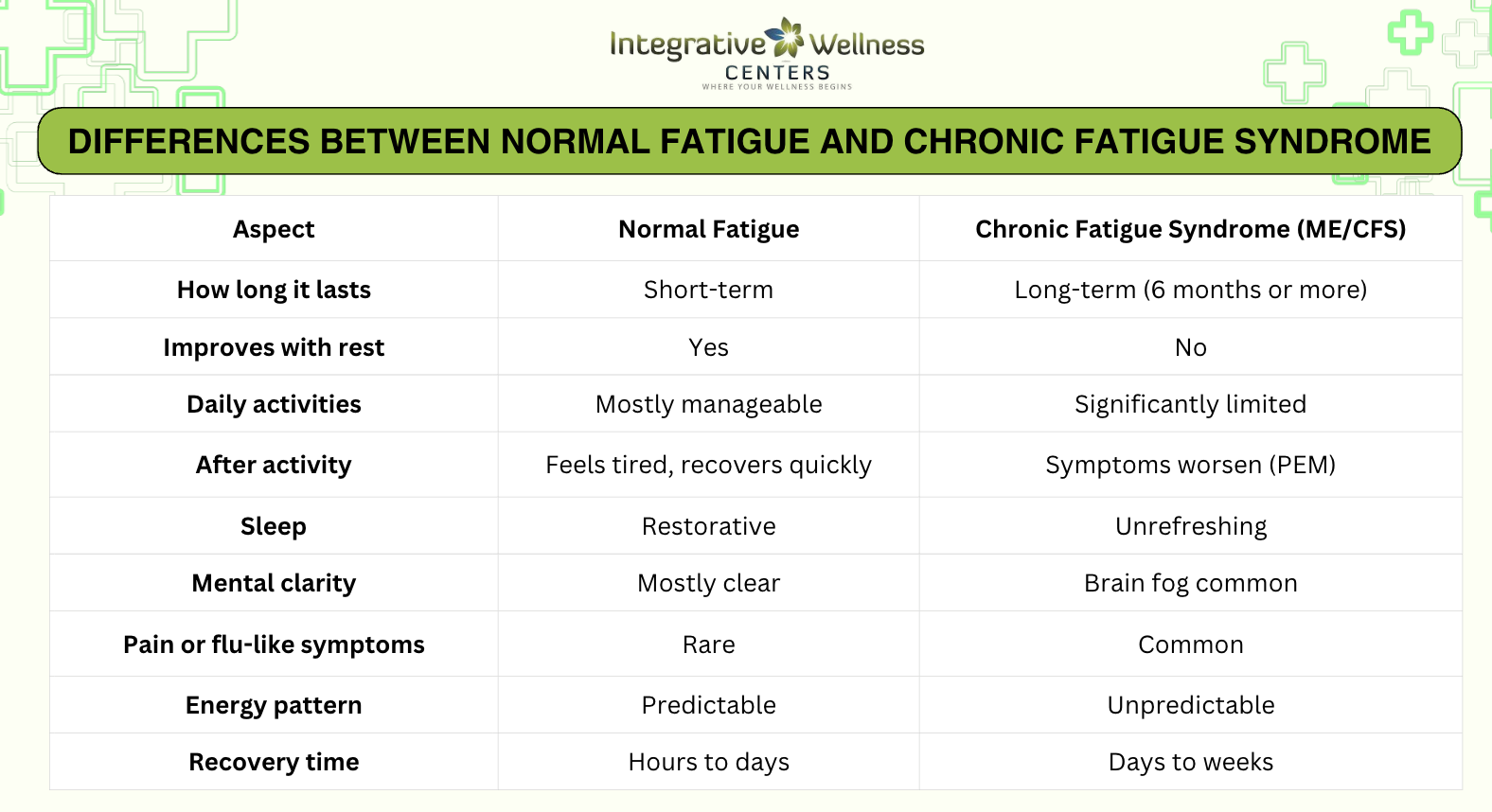
Unlike normal fatigue, the exhaustion seen in ME/CFS does not improve with rest. In fact, symptoms can worsen after even small amounts of physical, mental, or emotional effort. This makes everyday tasks such as working on a computer, socializing, or running errands feel overwhelming and unpredictable.
Key features commonly discussed in clinical sources include:
What truly defines ME/CFS is post-exertional malaise. This means symptoms may flare up hours or even days after activity, not immediately. Because of this delayed response, many people with ME/CFS feel trapped in a cycle of doing too much on a “good day” and then crashing afterward. Understanding this pattern is essential for proper management and long-term stability.
Read more Natural Treatments That Help Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome affects each person differently, and symptoms can change from day to day. Some people may appear functional on the outside while feeling completely depleted on the inside. Others may experience periods where even basic daily tasks feel overwhelming. This unpredictability is one of the most challenging aspects of ME/CFS.
Symptoms often involve multiple body systems at the same time, which is why people with ME/CFS may struggle to explain how they feel or why they cannot simply “push through” their fatigue.
Common symptoms experienced by people with ME/CFS include:
What makes these symptoms especially difficult is how they can fluctuate. A person may feel relatively stable one day and significantly worse the next, often without an obvious reason. This fluctuation is commonly linked to post-exertional malaise, where symptoms intensify after physical, mental, or emotional effort. Recognizing these symptom patterns helps guide safer daily routines and more effective long-term care.
Read more What is Chronic Fatigue Treatment and Where to Find it in Michigan
People living with ME/CFS often notice that symptoms do not worsen randomly. Flare-ups, sometimes called crashes, are usually triggered by specific physical, mental, or emotional stressors. The challenge is that these triggers are not always obvious at first, and symptoms may appear hours or even days later.
Understanding what triggers flare-ups is essential because it allows you to prevent crashes rather than constantly reacting to them. Over time, recognizing these patterns helps you make safer choices and build routines that support more stable energy.
What makes ME/CFS particularly difficult is that triggers often stack together. For example, a busy day that includes poor sleep, emotional stress, and physical activity may lead to a much stronger crash than any one factor alone. Because symptoms can be delayed, keeping track of activities and how you feel afterward can help identify personal triggers and prevent future flare-ups.
Read more Overcoming Fatigue: Understanding Stress Syndrome and Natural Solutions
Managing ME/CFS is not about pushing harder or becoming more disciplined. In fact, pushing through symptoms often makes things worse. The goal is to reduce flare-ups by protecting your limited energy and helping your body recover more consistently.
These strategies help keep your nervous system from becoming overloaded. When the body is constantly pushed past its limits, symptoms tend to worsen and recovery takes longer. By slowing down and respecting your energy boundaries, you give your body a better chance to stabilize and reduce the frequency and intensity of flare-ups over time.
Nutrition for ME/CFS is about stabilizing energy, reducing inflammation, and supporting digestion and the nervous system. There is no single “ME/CFS diet,” but many people feel better when they focus on gentle, nourishing foods.
These foods help maintain steady blood sugar and provide nutrients needed for energy production and immune balance. Many people with ME/CFS feel worse when meals are skipped or heavily processed foods dominate the diet.
Food tolerance varies widely. A food journal can help identify what supports your energy versus what triggers symptoms.
With ME/CFS, how you move matters more than how much you move. The goal is to support circulation, flexibility, and mental health without triggering post-exertional malaise (PEM).
These activities are most helpful when done in small amounts and stopped before fatigue sets in. Using a timer and resting afterward can help prevent crashes.
Consistency is more important than intensity. Many people with ME/CFS do best with brief, repeatable activities rather than longer sessions that lead to crashes.
Read more Chronic Fatigue Treatment with Functional Medicine Doctor
There is no single cure for Chronic Fatigue Syndrome (ME/CFS), which is why treatment works best when it focuses on the whole person rather than just symptoms. Because ME/CFS affects energy, sleep, digestion, hormones, immunity, and the nervous system, a functional medicine approach is often one of the most effective ways to manage the condition.
A functional medicine doctor looks for underlying contributors to fatigue, such as nutrient deficiencies, digestive imbalance, hormone disruption, immune stress, and lifestyle factors. Instead of using a one-size-fits-all plan, care is personalized to your symptoms, history, and current capacity. This approach also emphasizes pacing, sleep support, nutrition, and stress regulation to help reduce flare-ups and improve daily functioning over time.
Read more Natural Treatments That Help Chronic Fatigue Syndrome (CFS)
Integrative Wellness Centers offers functional medicine care for people with chronic fatigue in Michigan, with options for online consultations as well. Their team works with patients experiencing ME/CFS and related conditions such as digestive issues, hormonal imbalance, and immune dysfunction, using a personalized and supportive approach.
If you’re ready to explore a root-cause approach to chronic fatigue, you can schedule an appointment with Integrative Wellness Centers at https://www.iwcenters.com/.
Chronic Fatigue Syndrome (ME/CFS) requires a personalized, whole-body approach rather than a one-size-fits-all treatment. Functional medicine focuses on identifying and addressing root contributors such as sleep disruption, digestive imbalance, hormone dysfunction, immune stress, and lifestyle factors while emphasizing pacing and recovery. By treating the underlying patterns that drive fatigue, functional medicine can help reduce flare-ups, improve daily function, and support long-term stability.
Common symptoms include persistent, severe fatigue that does not improve with rest, post-exertional malaise (worsening symptoms after activity), unrefreshing sleep, brain fog, muscle or joint pain, headaches, dizziness, and sensitivity to light or sound.
Early signs often include ongoing exhaustion after minor activity, frequent crashes, difficulty concentrating, sleep that doesn’t feel restorative, and feeling worse after physical or mental effort.
Triggers may include viral or bacterial infections, physical or emotional stress, sleep disruption, overexertion, immune stress, hormonal imbalance, or significant life events. Triggers can vary by person.
A crash often feels like sudden, overwhelming exhaustion with worsened pain, brain fog, flu-like symptoms, and an inability to function. Symptoms may appear hours or days after activity and can last days or weeks.
Some people experience improvement over time, especially with proper pacing and supportive care. Others may have long-term symptoms. There is no guaranteed cure, but symptoms can often be better managed.
For some people it is long-term, while others improve significantly. Early recognition, pacing, and personalized care can improve outcomes and quality of life.
Yes. ME/CFS does not typically shorten life expectancy, but it can significantly affect quality of life if not managed properly.
No. There is no single blood test that diagnoses ME/CFS. Doctors use symptom criteria and testing to rule out other conditions that cause fatigue. Schedule your consultation with our Functional Medicine Doctor to know more about Chronic Fatigue Syndrome
Diagnosis is based on symptoms lasting six months or longer, presence of post-exertional malaise, unrefreshing sleep, and reduced daily functioning, while ruling out other medical causes.
Care may involve primary care physicians, functional medicine doctors, integrative medicine practitioners, and specialists depending on symptoms. Functional medicine doctors often coordinate care across systems.
There is no single best treatment. The most effective approach is personalized care that includes pacing, sleep support, nutrition, stress regulation, and addressing root contributors through functional medicine.
Doctors can rule out other conditions, help manage symptoms, guide pacing strategies, address sleep issues, and identify contributing factors such as nutrient deficiencies or hormone imbalance.
Many people choose to limit ultra-processed foods, refined sugar, excess caffeine, alcohol, and foods that personally trigger symptoms or digestive issues.
Deficiencies in vitamin B12, vitamin D, iron, magnesium, and folate can contribute to fatigue. Testing and guidance from a clinician is recommended before supplementing.
Coffee can worsen symptoms for some people by overstimulating the nervous system or disrupting sleep. Tolerance varies by individual.
Yes. ME/CFS can affect children and adolescents, often following infections, and may significantly impact school and daily activities.
You should seek medical evaluation if fatigue lasts more than a few weeks, interferes with daily life, worsens after activity, or is accompanied by symptoms like dizziness, pain, brain fog, or sleep problems.

Take the online digestive evaluation to instantly discover what systems of your body are the cause of your health issues.
Online Digestive EvaluationTake the TestOnline Female Hormone EvaluationOnline Male Hormone Evaluation
When you sign up you'll receive free access to our Hormones Report, Program Guide and more.